Medical Marijuana 101: the science behind cannabis and its implications for patients
On Wednesday, October 24, the Columbus Medical Association (CMA) held its annual Emerging Trends in Healthcare program. This year’s topic was “Marijuana as Medicine: What Clinicians Want to Know About the Science.”
Three experts – doctors Gary Wenk (PhD), Jerry Mitchell (MD), and Harrison Weed (MD) – each provided an overview of the research behind medical marijuana, expanding on its implications for physicians and their patients.
Their full presentations can be accessed by CMA members at the following link:
”Marijuana as Medicine” (full-length podcast)
Dr. Jerry Mitchell presents at the CMA’s annual Emerging Trends in Healthcare program
While physicians can now recommend marijuana as a treatment option for their patients, the majority are hesitant to do so. There are relatively few clinical studies to guide doctors in their recommendations of CBD and THC products. Consequently, the availability of this drug has largely been driven by public demand, rather than medical research.
“There is no clinical data. What we have is anecdote, for the most part,” Dr. Wenk said.
Doctor Wenk, a Professor of Psychology & Neuroscience at the Ohio State University, has conducted extensive preclinical research on marijuana’s neurological effects. According to Dr. Wenk, marijuana holds promise for the treatment of pain, inflammation, and degenerative diseases. Of course, the supporting research has largely been constrained to animal populations.
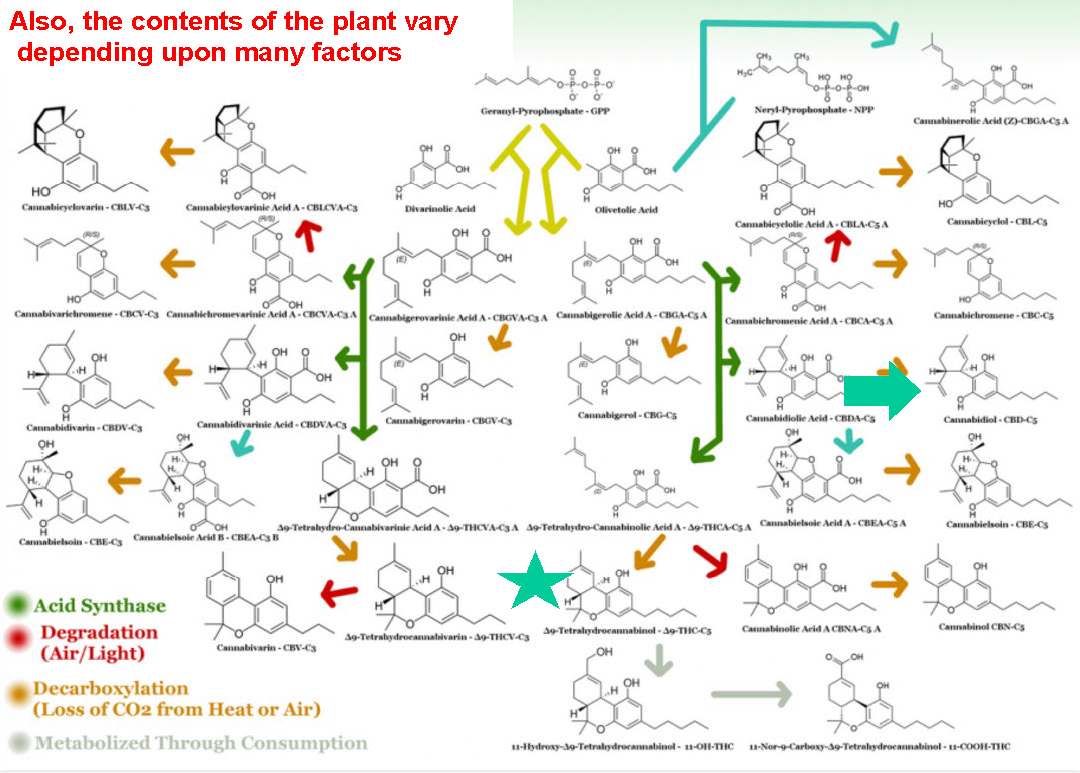
“When your patient asks you; what’s this going to do to me? The answer is, lots of things, and I can’t explain all of them,” Dr. Wenk said. “How you experience marijuana is determined by what’s in the plant. This is the same as saying whatever’s in the little white pill that you get at CVS will determine what that drug is going to do.”
According to Dr. Wenk, sample consistency can be a major issue in marijuana studies. The plant strains used in medical research may not be representative of plant varieties available on the consumer market. Doctor Mitchell says this issue is equally troubling on the clinical side of research.
“You’re not going to have a pure study because you’re not going to have a pure product,” Dr. Mitchell said. “You don’t know how it was handled, you don’t know where their supply was. It is a real challenge to interpret any of these studies.”
In the United States, the only institution certified to supply marijuana plant material for medical research is the University of Mississippi. This means that study results are representative only of the strains that the University of Mississippi chooses to grow.
In Ohio, marijuana cultivators, producers, and testing companies are regulated by the U.S. Department of Commerce; while dispensaries are regulated by the State Board of Pharmacy.
Photo by Get Budding on Unsplash
Presently, physicians are not permitted to prescribe marijuana in the state of Ohio. However, they may recommend it to patients. To become a recommender, one must first obtain an endorsement on their medical license from the State Medical Board. More information on this process can be found here, on the Ohio Medical Marijuana Control Program website.
In Ohio, marijuana has been approved for these 21 conditions. While a number of FDA-Approved cannabinoids currently exist, Dr. Wenk cautions that different kinds of marijuana-based products can have very different effects, depending on each product’s specific blend of cannabinoid-compounds.
“Many of these compounds act on the body and brain,” Dr. Wenk said. “Whether they act upon you depends on what you’re using. Are you using marijuana? Are you using an oil? Are you eating hundreds of milligrams of it?”
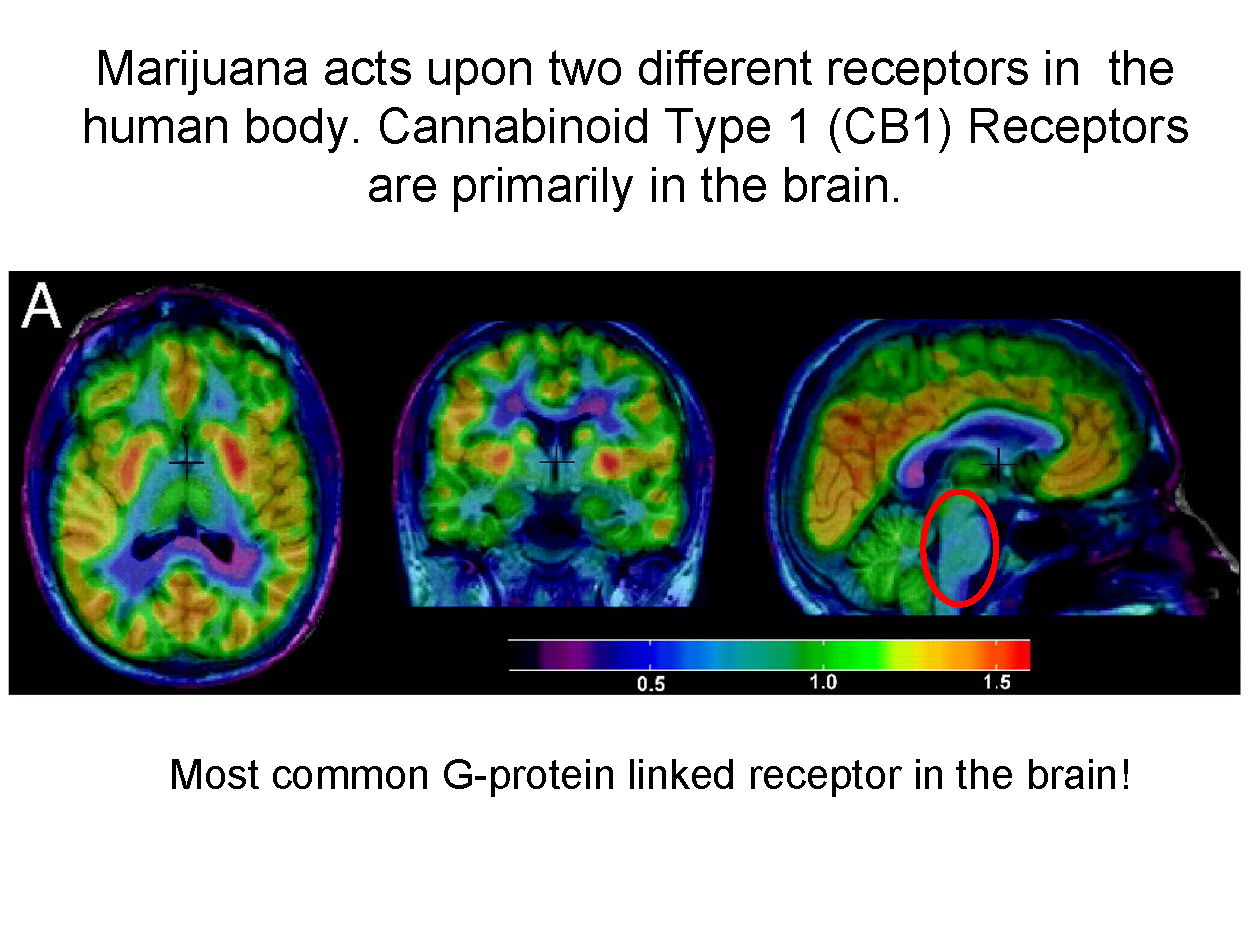
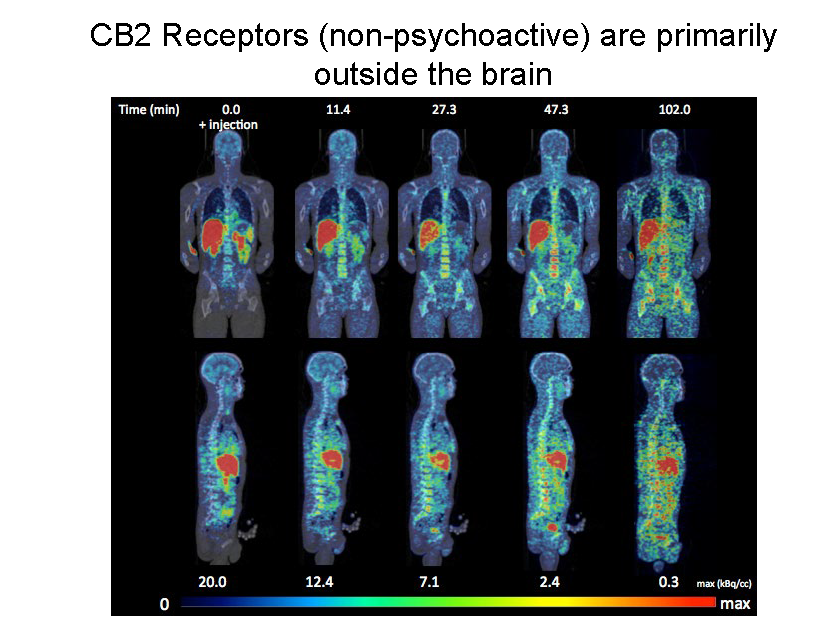
The primary cannabinoid compounds in marijuana are THC and CBD. The ratio (and concentration) of these two compounds will largely determine the effects that a given product will have on the user. By signaling the body’s CB1 and CB2 receptors, marijuana can trigger a variety of psychological and physiological responses.
“(CB1 receptors) are everywhere in the brain. It’s the most common g-protein system we have in the brain. This makes interpreting what the drugs are going to do especially difficult,” Dr. Wenk said. “It’s in places that will affect how people hear, see, think and feel.
Until cannabis is better understood through clinical studies, physicians are unlikely to embrace it as a proper substitute for prescription medications. While many patients are turning to cannabis as an alternative to opioids, stimulants, and antidepressants – doctors are erring on the side of caution.
“I want us to move cautiously because I don’t want marijuana to be the opioid epidemic of the future,” Dr. Ahmad Mostafavifar said.
Dr. Mostafavifar, a hospitalist at the Ohio State Wexner Medical Center, says there are a “select few” patients who stand to benefit from medical marijuana. He fears that financial interests have driven the drug to be marketed as a broad solution for many conditions – without evidence that it truly works for those conditions.
“This is what we did with oxycodone in the 1990s. Everybody was profiting from it, the pharmaceutical companies… and we definitely see a hint of that now with marijuana,” he said.
Dr. Liz Lottes, retired family practitioner with experience in addiction medicine, echoes these concerns. She pointed out that, even though the state legislature has approved marijuana’s use for a list of conditions, there are no randomized controlled studies solidly indicating their effectiveness in treating those conditions.
“Physicians rely on data and research from trials before using new medications,” Dr. Lottes explained. “Currently there are none supporting marijuana other than the previous forms such as Marinol.”
There are also concerns over marijuana’s potential side effects, which can include impaired judgement, impaired memory, immunosuppression, psychosis, dizziness, dysphoria, nausea, decreased fertility, and neurodevelopmental disorders in children.
“As physicians, we're trying to figure out how to navigate these new waters because these are pretty much uncharted territories for us,” Dr. Jeffrey Janis, CMA President, said. “Our patients are going to come to us with questions and we need to be prepared to answer them."
For more information about medical marijuana in Ohio, visit https://www.medicalmarijuana.ohio.gov/.



